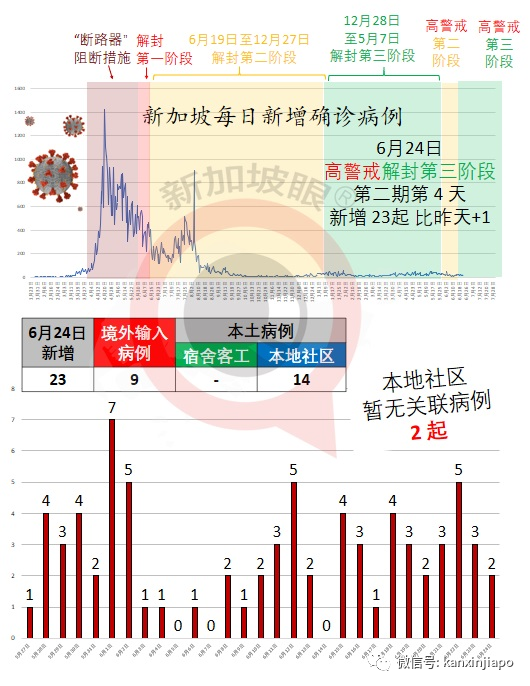
6月24日,新加坡衛生部通報初步統計:今天新增確診23例,累計6萬2493例。新增病例當中,境外輸入9起,本土病例14起,皆爲本地社區病例,客工宿舍病例無新增;在14起本土病例當中,12起是有關聯病例,其中11人在隔離狀態下確診,1人是在當局積極檢測中被發現的;另有2起爲暫無關聯病例。衛生部將在今晚公布詳情。

我們也正在和疫苗制造商合作,希望能讓疫苗提前抵達新加坡,並加快我國人口接種疫苗的速度。 臨床數據清楚證明,疫苗在降低感染冠病和病毒傳染的風險方面非常有效。即使染病,疫苗也能預防患者出現嚴重症狀。 在以色列,未接種疫苗者的染病率比已接種疫苗者高30倍,住院率相比起來也高10倍。 在新加坡,有120多人接種兩劑疫苗後仍感染冠病,當中包括65歲以上但不住在醫院或療養院的年長者,他們都沒有出現任何症狀,或僅出現輕微症狀。相比之下,未接種疫苗的冠病患者當中,約有8%出現嚴重症狀。 未來,我們可能讓國人接種追加劑,以讓大家能繼續獲得高度保護,同時也能預防新變種毒株對現有疫苗産生抵抗力。因此,我們可能必須實行一項能夠持續多年的全面疫苗接種計劃。 




有了長期的疫苗接種計劃、更簡易、更全面的檢測、更有效的治療方法,再加上大家都負起社會責任,這可能意味著在不久的將來,當有人患上冠病時,我們的應對措施就可能會與現在大不相同。
?(新加坡衛生部長王乙康與新加坡演藝圈阿姐鄭惠玉拍防疫視頻,以上圖源:王乙康臉書) 新常態可能會是這樣的: 輕症病患不住院 首先,病患可以在家中康複,因爲接種了疫苗的人一般只會出現輕微的症狀。由于病患身邊的人也都接種了疫苗,傳播風險也會減低,所以我們也不會太擔心醫療系統不堪重負。 不大規模追蹤密接者 第二,每當我們發現有人受感染時,也許不必大規模追蹤密切接觸者,以及將人們隔離開來。人們可以定期使用各種快速簡易的方式自行檢測。如果檢測結果呈陽性,他們可以通過PCR檢測加以確認,然後自我隔離。 只監測重症情況 第三,我們將不再著重監測每天的患病人數,而是把焦點放在有多少人患重病、有多少人在加護病房留醫、有多少人須接受插管治療等方面的數據。這就和我們現在監測流感的方式一樣。 恢複大型活動 第四,我們可以逐步放寬安全管理措施,恢複大型的聚會和活動,如國慶慶典或新年倒數活動。各企業也能確信,它們的運作不會受到幹擾。 
第五,我們將可以再次出國旅遊,至少能去那些同樣已將疫情控制下來、冠病成爲地方性常態的國家。我們將相互承認對方的疫苗接種證書。旅客也可以在出境前接受檢測,抵境時的冠病檢測結果若是陰性,就無須隔離,尤其是已經接種疫苗的旅客。

向上滑動閱覽
Living normally, with Covid-19
We are continuing with our efforts to control the worrisome Delta variant of Covid-19. Given its high transmissibility, it will be hard to bring infections down to zero. Instead, we are adopting an aggressive ring-fencing strategy-casting a wide net to isolate contacts of infected persons, and testing tens of thousands every day. The aim is to minimise the risk of large clusters forming.
But it has been 18 months since the pandemic started, and our people are battle-weary. All are asking: When and how will the pandemic end?
Endemic Covid-19
The bad news is that Covid-19 may never go away. The good news is that it is possible to live normally with it in our midst. This means Covid-19 will very likely become endemic. But what does that mean?
It means that the virus will continue to mutate, and thereby survive in our community. One example of such an endemic disease is influenza. Every year, many people catch the flu. The overwhelming majority recover without needing to be hospitalised, and with little or no medication. But a minority, especially the elderly and those with co-morbidities, can get very ill, and some succumb.
In a large country, the number hospitalised from influenza can be huge. For example, in the United States, hundreds of thousands are hospitalised every year because of the flu, and tens of thousands die.
But because the chances of falling very ill from influenza are so low, people live with it. They carry on with their daily activities even during the flu season, taking simple precautions or getting an annual flu jab.
We can work towards a similar outcome for Covid-19. We can’t eradicate it, but we can turn the pandemic into something much less threatening, like influenza, hand, foot and mouth disease, or chicken pox, and get on with our lives.
Doing so will be our priority in the coming months. We already have a broad plan.
Vaccination is key
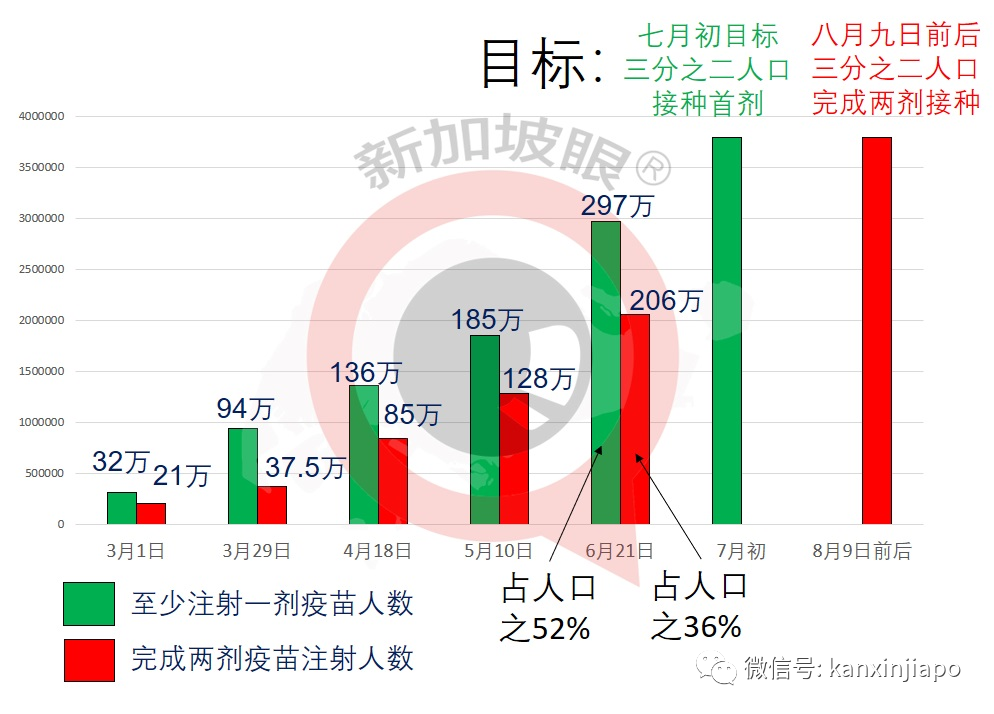
First, vaccination. During his broadcast on May 31, the Prime Minister said we aimed to have two-thirds of our population take at least their first dose by early July. We are on track to achieve that target. Our next milestone will be to have at least two-thirds of our population fully vaccinated with two doses around National Day, supply permitting.
We are working to bring forward the delivery of vaccines and to speed up the process.
The evidence is clear: Vaccines are highly effective in reducing the risk of infection as well as transmission. Even if you are infected, vaccines will help prevent severe Covid-19 symptoms.
Israel’s experience shows that the infection rate among vaccinated persons is 30 times less than that of the unvaccinated. The hospitalisation rate for the vaccinated is also lower by 10 times.
In Singapore, of the 120 plus fully vaccinated individuals who were nevertheless infected with Covid-19, including some aged above 65 and were not resident at hospitals or nursing homes – all had either no or mild symptoms. In contrast, about 8 percent of the unvaccinated developed serious symptoms.
To sustain a high level of protection, and to defend against new mutant strains resistant to current vaccines, booster shots may be needed in the future. We may have to sustain a comprehensive, multi-year vaccination programme.
Early evidence suggests that with vaccination, we can tame Covid-19. Again, the experience of Israel – which has vaccinated
60 per cent of its population, the highest vaccination rate in the world currently is pertinent.
Across all age groups, the hospitalisation rate due to Covid-19 in Israel among those fully vaccinated is 0.3 per 100,000 persons daily, and the mortality rate is 0.1 per 100,000 persons.
In comparison, in 2018/19, the hospitalisation and mortality rates for influenza in the US were 0.4 and 0.03 per 100,000 persons daily, respectively. In a severe flu season, like in 2017/18, the rates were 0.67 and 0.05, respectively.
Essentially with a high rate of vaccination, Israel has brought the clinical outcomes of Covid-19 close to that of seasonal influenza in the US. These are very promising outcomes.
Testing will be easier
Second, testing and surveillance will still be needed, but the focus will be different. We would still need rigorous testing at our borders to identify any person carrying the virus, especially variants of concern.
Domestically, testing will be less of a tool for ring-fencing and quarantining people exposed to infected persons. Instead, it would be to ensure that events, social activities and overseas trips can take place safely; as well as to reduce transmission risks, especially to those who are vulnerable to infections.
We cannot rely only on the polymerase chainreaction (PCR) test, which can be uncomfortable and takes many hours to produce results. We need to make Covid-19 testing fast and easy. We have rolled out antigen rapid tests, including self-tests, to polyclinics, private clinics, employers, premises owners and pharmacies.
There are even faster test kits in the pipeline, such as breathalysers, that take about one to two minutes to produce the results and do not involve swabbing. In time, the airport, seaport, office buildings, malls, hospitals and educational institutions can use these kits to screen staff and visitors.
There is also waste water testing, which is useful to find out if there are hidden infections in dormitories, hostels or housing estates.
Treatments will improve
Third, scientists around the world are working on treatments for Covid-19. Today, we already have a range of effective treatments, which is one reason why Singapore’s Covid-19 mortality rate is among the lowest in the world.
Eighteen months after the pandemic started, we now have many therapeutic agents that are effective in treating the critically ill, quickening recovery, and reducing disease progression, severity and mortality. The Ministry of Health tracks these developments closely, ensuring that we have adequate supplies of these drugs. Our medical researchers actively participate in the development of new treatments.
Social responsibility remains critical
Finally, whether we can live with Covid-19 depends also on Singaporeans’ acceptance that Covid-19 will be endemic and our collective behaviour.
If all of us practise good personal hygiene, we are less likely to be infected. If all of us are considerate to one another, staying away from crowds when we feel unwell, we will reduce transmission. I fall of us shoulder the burden together – workers keeping their colleagues safe by staying at home when ill, and employers not faulting them – our society will be so much safer.
Towards a new normal
With vaccination, testing, treatment and social responsibility, it may mean that in the near future, when someone gets Covid-19, our response can be very different from now.
The new norm can perhaps look like this:
First, an infected person can recover at home, because with vaccination the symptoms will be mostly mild. With others around the infected person also vaccinated, the risk of transmission will be low. We will worry less about the healthcare system being overwhelmed.
Second, there may not be a need to conduct massive contact tracing and quarantining of people each time we discover an infection. People can get themselves tested regularly using a variety of fast and easy tests. If positive, they can confirm with a PCR test and then isolate themselves.
Third, instead of monitoring Covid-19 infection numbers every day, we will focus on the outcomes: how many fall very sick, how many in the intensive care unit, how many need to be intubated for oxygen, and so on. This is like how we now monitor influenza.
Fourth, we can progressively ease our safe management rules and resume large gatherings as well at major events, like the National Day Parade or New Year Countdown. Businesses will have certainty thattheir operations will not be disrupted.
Fifth, we will be able to travel again, at least to countries that have also controlled the virus and turned it into an endemic norm. We will recognise each other’s vaccination certificates. Travellers, especially those vaccinated, can get themselves tested before departure and be exempted from quarantine with a negative test upon arrival.
We are drawing up a road map to transit to thisnew normal, in tandem with the achievement of our vaccination milestones, though we know the battle against Covid-19 will continue to be fraught with uncertainty.
In the meantime, we still need to take the necessary precautions and safeguards, to keep infections and hospitalisations at bay.
History has shown that every pandemic will run its course. We must harness all our energy, resources and creativity to transit as quickly as we can to the desired end-state. Science and human ingenuity will eventually prevail over Covid-19. Cohesion and social consciousness will get us there faster. We must all do our part.